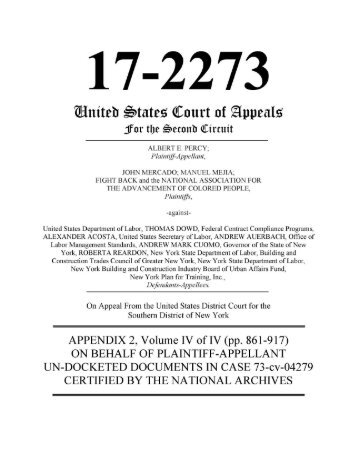
The Percy Program
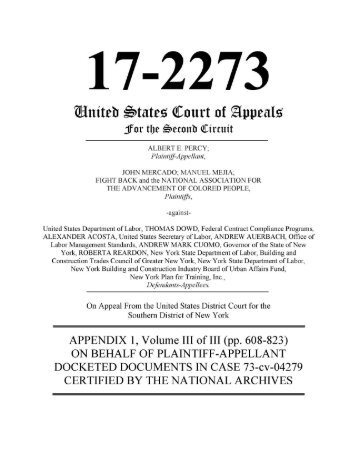
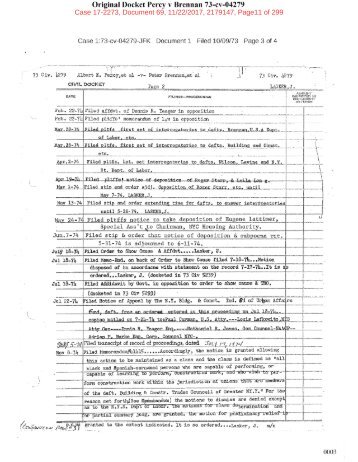
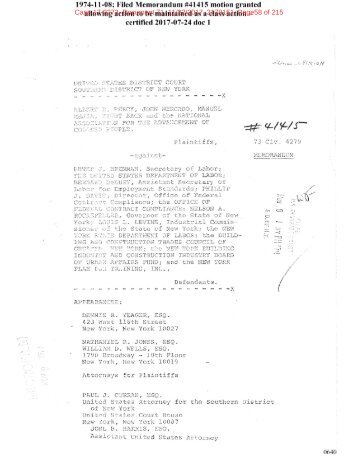
It is a fight to level the playing field to be able to compete for jobs and careers on the basis of skills and make available apprentice training to all. In 1973 Al Percy launched a class action lawsuit to give workers like him a chance to better their lot in life. It would also ensure the availability of skilled workers to build the infrastructure of the future.
Attachment 5 EDNY Percy v Employer and Owners 21-cv-01366 Attachment #1 NYS AG Report
- Text
- Nursing
- Residents
- Homes
- Staffing
- Facilities
- Resident
- Deaths
- Guidance
- Reported
- Pageid
- Attachment
- Edny
- Percy
- Employer
- Owners
Case
Case 1:21-cv-01366-NGG-SJB Case MDL No. 3011 Document 1-1 25-5 Filed Filed 03/15/21 06/24/21 Page Page 40 40 of 83 of 83 PageID #: 137 Admissions Decisions and Staffing Decisions: A facility’s decision to admit new residents is also a staffing decision because it requires a facility to assess whether its staffing level is sufficient to provide care to meet the needs of the existing residents and any proposed new residents. When a for-profit nursing home has an empty bed, it has a financial motivation to increase its census by admitting residents in order to obtain the daily rate of reimbursement offered by the resident’s payor – Medicaid, Medicare, other federal health insurance, or private insurance. 56 During the pandemic, many facilities experienced empty beds as residents died from COVID-19 or other causes. Some families took their loved ones to a family member’s home. A decrease statewide in elective surgeries at hospitals reportedly stopped a regular flow of patients to nursing homes for rehabilitation. As discussed above, many facilities also experienced staffing reductions due to COVID-19 illness and quarantine, which necessarily decreased the facility’s capacity to provide care for its residents, and, as the examples discussed herein reflect, resulted in exacerbated staffing problems. The preliminary investigations indicate that nursing homes took a variety of approaches to decisions to admit residents during the COVID-19 pandemic, even as they were experiencing staffing shortages due to staff illness from, or otherwise inability to work due to, COVID-19. The approaches suggest admissions decisions were affected to varying degrees by financial motives, and by clinical and administrative evaluations of the facility’s ability to provide appropriate care to its residents. OAG received information during its investigations that some facilities decided that the safest course was to stop admitting residents for periods of time while their staffing was low. For example, a not-for-profit nursing home in New York City with CMS 2-Star Staffing and 3- Star Overall ratings that experienced staffing shortages due to COVID-19 infection reported that it stopped admissions on March 21 due to 20 percent of staff calling in sick. In addition, to improve staffing, the facility brought in agency staff home health aides and restructured the staff. In contrast, a for-profit nursing home in Western New York with CMS 1-Star Staffing and 1-Star Overall ratings indicated it took a different approach to admissions. Managers at that facility alleged that as of the end of April, the facility continued to accept new residents despite ongoing staffing difficulties, having nine out of 126 residents who tested positive for COVID-19, five residents dying from confirmed COVID-19, and five staff testing positive for COVID-19. A for-profit facility in Western New York with CMS 2-Star Staffing and 2-Star Overall ratings indicated it also accepted new patients in April, but only admitted residents if they had recovered from COVID-19. However, as of April 30, according to a nurse supervisor, the facility was not taking admissions for at least a week due to the “state of the facility.” The investigation reflected that the “state of the facility” included unstable conditions as alleged by staff: 40
Case 1:21-cv-01366-NGG-SJB Case MDL No. 3011 Document 1-1 25-5 Filed Filed 03/15/21 06/24/21 Page Page 41 41 of 83 of 83 PageID #: 138 » A high rate of COVID-19 positive cases, with 33 out of 59 residents testing positive; » The facility had tested less than half of the residents; » The facility did not have enough tests to test the remaining residents, and was trying to get more; » 14 positive staff members and 12 more pending staff tests; » Staffing shortages; » The facility administrator was out sick. As of mid-May, the nurse supervisor asserted that staffing had improved, with most staff who were out sick or quarantined returning to work. As of the following week, the acting administrator advised that staffing issues were continuing to improve, testing issues had been resolved, and facility had been COVID-19 free for two weeks, and facility expected to be taken “off precautions” from DOH shortly. The facility provided documentation indicating it had passed DOH infection control surveys in early May and mid-May. Financial Incentives Illustration — Admissions: As illustrated in the example below, the preliminary investigations reflect how the financial incentives within the current system resulted in pressure by some for-profit owners to push staff to admit increased numbers of residents from hospitals in order to reach census goals, regardless of whether the facility had sufficient staff to care for them. Specifically, in one for-profit facility in New York City with CMS 2-Star Staffing and 1-Star Overall ratings, an administrator reported communications with an owner about hospital admissions. The facility interpreted DOH’s March 25 guidance not to deny admission of residents from the hospital solely on the basis of a COVID-19 positive diagnosis as “they were to admit COVID-19 residents from the hospital.” The facility admitted five hospital patients on March 26, but the owners wanted to admit more. The administrator alleged that there were arguments with the owners over how many residents they could safely care for. According to the administrator, every new admission from the hospital was a patient who was “COVID positive.” 57 Incentive Pay and Bonuses to Staff: Preliminary investigative findings also reflected a range of sizes of financial investment that facilities and/or owners were willing to make for short periods of time during the pandemic to provide monetary incentives to health care workers in order to retain staff, to attract new staff as full-time employees or as temporary agency staff, and to encourage staff to work additional shifts at the facility. Facilities’ reported choices in providing financial incentives to increase staffing reflect different perspectives on what level of expenses were determined to be necessary versus optional. Some facilities paid small bonuses to staff for each additional shift they took, with some limiting the bonus to shifts involving work with COVID-19 positive residents. Other facilities paid generous salary increases per hour for hazard pay. Still other facilities paid staff both salary increases and bonuses per extra shift worked. Some offered hazard pay for a few weeks, while others offered it for longer periods of time. Some paid agency staff extra, while others did not. 41
- Page 1 and 2: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 3 and 4: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 5 and 6: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 7 and 8: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 9 and 10: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 11 and 12: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 13 and 14: Guidance Issued by Federal and Stat
- Page 15 and 16: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 17 and 18: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 19 and 20: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 21 and 22: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 23 and 24: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 25 and 26: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 27 and 28: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 29 and 30: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 31 and 32: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 33 and 34: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 35 and 36: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 37 and 38: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 39: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 43 and 44: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 45 and 46: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 47 and 48: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 49 and 50: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 51 and 52: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 53 and 54: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 55 and 56: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 57 and 58: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 59 and 60: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 61 and 62: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 63 and 64: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 65 and 66: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 67 and 68: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 69 and 70: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 71 and 72: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 73 and 74: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 75 and 76: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 77 and 78: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 79 and 80: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 81 and 82: Case 1:21-cv-01366-NGG-SJB Case MDL
- Page 83: Case 1:21-cv-01366-NGG-SJB Case MDL
Inappropriate
Loading...
Mail this publication
Loading...
Embed
Loading...